Accurate electrocardiogram (ECG/EKG) readings start with proper electrode positioning. For biomedical equipment technicians and clinical engineering teams, understanding 3 lead EKG placement is essential—not only for validating device performance but also for training clinical staff and troubleshooting reported issues. Even minor misplacements can affect diagnostic accuracy, trigger false alarms, and lead to unnecessary follow-up tests.
Why Electrode Placement Matters
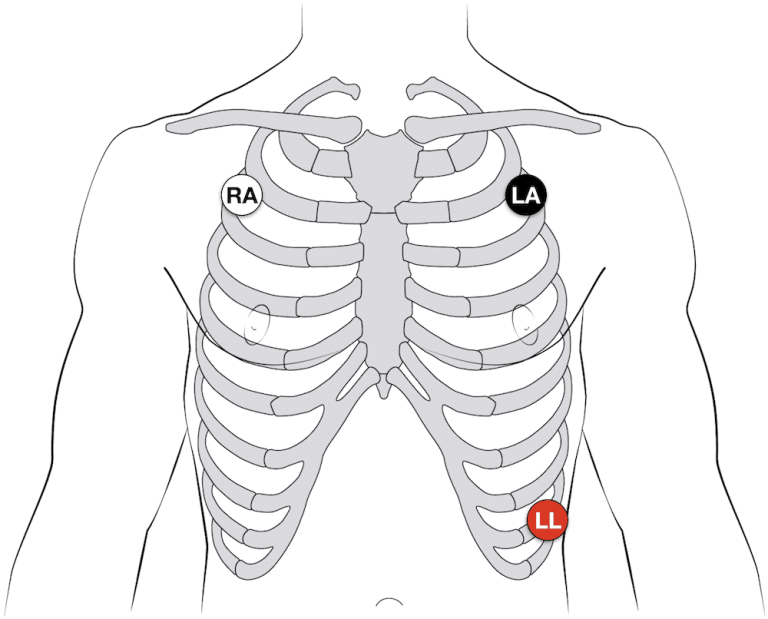
The 3-lead configuration is one of the most common in hospital monitoring, especially for continuous bedside telemetry or during transport. With only three electrodes—right arm (RA), left arm (LA), and left leg (LL)—the system produces a simplified tracing of heart activity. While it doesn’t provide as much data as a 12-lead, it’s critical for rhythm analysis and patient safety. If electrodes are applied incorrectly, the waveform morphology can change, making it difficult for clinicians to interpret or for devices to alarm appropriately.
Anatomical Landmarks for 3-Lead Placement
To achieve reliable readings, technicians should verify that electrodes are placed over clean, dry skin and at consistent landmarks:
- Right Arm (RA): Just below the right clavicle near the deltoid muscle.
- Left Arm (LA): Just below the left clavicle near the deltoid muscle.
- Left Leg (LL): On the lower torso, often the left lower abdomen, away from major muscle movement.
This triangular arrangement approximates Einthoven’s triangle, the basis for deriving Lead I, II, and III signals.
Skin Preparation and Lead Quality
Signal quality begins with skin preparation. Oils, sweat, and hair can interfere with electrode adhesion and conductivity. Best practices include:
- Shaving excess hair at electrode sites.
- Cleaning skin with alcohol or mild soap and water.
- Allowing skin to dry fully before applying electrodes.
Technicians performing acceptance testing or preventive maintenance on monitors should confirm that the electrodes used in demonstrations are fresh and within expiration dates.
Common Errors in 3-Lead Placement
Even experienced staff can make mistakes when hurried or distracted. Some of the most frequent issues include:
- Swapped Electrodes: RA and LA leads reversed can invert waveforms.
- Placing LL on an Arm: Leads to abnormal axis and misinterpretation.
- Too Close Together: Reduced amplitude and distorted tracings.
Biomedical equipment teams can help mitigate these errors by incorporating correct diagrams into user training and by labeling cables clearly.
Integration With Patient Monitors
From a technical standpoint, biomedical technicians must ensure that the patient monitor’s input circuitry is functioning properly. This involves checking lead wires for continuity, inspecting connectors for corrosion, and verifying calibration. Understanding correct 3-lead placement helps technicians differentiate between a device fault and a user-related issue.
Training and Competency Support
Because clinical staff turnover is common, recurring education on lead placement is essential. Biomed departments can create quick-reference cards, laminated diagrams, or even QR codes on monitor carts linking to step-by-step instructions. In addition, technicians can verify signal quality on themselves or on test simulators to demonstrate proper placement during in-services.
Considerations for Special Populations
Certain patient groups present additional challenges:
- Pediatric Patients: Smaller chest area may require modified placement to maintain signal quality without interfering with medical devices.
- Burn or Wound Sites: Electrodes may need to be positioned in alternative but symmetrical locations to avoid compromised skin.
- High-Motion Environments: Transport monitors may require more secure electrodes or additional skin prep to maintain contact.
Being aware of these scenarios helps biomed teams provide better guidance to clinical staff and prevents unnecessary service calls.
Documentation and Compliance
Accurate records of preventive maintenance and performance testing should note not only the monitor’s functional status but also the type of leads used and their placement during testing. This documentation can be vital for accreditation inspections and for resolving future questions about equipment performance.
Why Mastery of 3-Lead Placement Benefits Biomed Teams
When technicians are proficient in 3-lead EKG placement, they can:
- Rapidly troubleshoot signal quality complaints.
- Support clinicians with accurate guidance.
- Reduce downtime of monitoring equipment.
- Contribute to improved patient care and safety.
It’s a core competency that enhances credibility and effectiveness in the healthcare technology management (HTM) field.
Whether you’re onboarding new monitors, validating accessories, or educating nursing staff, mastering correct electrode positioning is an indispensable skill for every biomedical technician. For trusted resources, parts, and expert support to keep your monitoring equipment performing at its best, explore THE BIOMED GUYS—your partner in biomedical equipment service, repair, and sourcing.